In the last 20 years, the number of American adults diagnosed with diabetes has doubled. Did you know that 37 million Americans have diabetes, and approximately 21% of those are unaware that they have it? Couple that statistic with the 96 million people considered “pre-diabetic,” and the number of individuals whose vision potentially could be affected by the disease is staggering.
Diabetes is the leading cause of blindness in patients under age 74; with early detection and treatment, diabetics can reduce their risk of going blind by 95%! Did you know that 20% of people first learn of their diabetic condition through a comprehensive eye exam? That’s one reason why an annual eye exam is so crucial to the health of your eyes.
- What is diabetes, and how does it impact vision?
Diabetes is a progressive, chronic disease that occurs when there is too much glucose, or sugar, in the blood. When blood sugar is elevated, the pancreas releases the hormone insulin, which turns blood sugar into energy that your cells can use. When the pancreas doesn’t produce enough insulin or the cells don’t respond to it (a condition called insulin resistance), glucose stays in the body’s bloodstream. Over time, this elevated sugar in the blood can cause serious health issues, including vision loss, cardiovascular issues, and kidney disease.
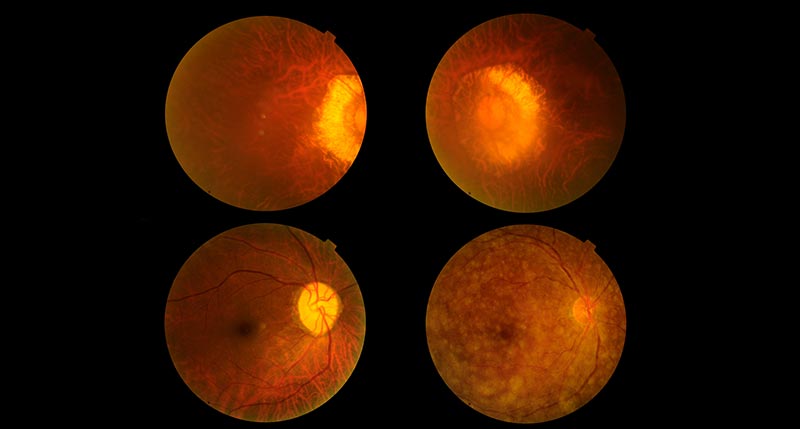
When blood sugar stays elevated over time, it damages the tiny, sensitive blood vessels in the back of the eye, causing swelling, scarring and high pressure within the eye. These changes can cause eye conditions, including diabetic retinopathy, diabetic macular edema, cataracts, and glaucoma.
Your optometrist examines the back of your eyes for vascular changes that can damage tissue and lead to Diabetic Eye Disease, which includes 4 conditions that can threaten your sight:
- Diabetic retinopathy impacts blood vessels in the retina (the light-sensitive layer of tissue in the back of the eye). Some blood vessels close off, causing new vessels to form on the retina — a condition called proliferative diabetic retinopathy. Associated symptoms include floaters, poor night vision, shadowy areas in the visual field, and double vision.
- Diabetic macular edema is a swelling of the macula — the small, sensitive area of the retina responsible for up-close and central vision. We need the macula in order to read, drive, and see people’s faces. Diabetes can destroy the sharp vision in this part of the eye.
- Glaucoma often damages the optic nerve, resulting in a slow loss of side vision and blindness if not treated early.
- Cataracts, a clouding of the eye’s natural lens, can be caused by deposit buildup from high glucose levels.
- What are the signs and symptoms of Diabetic Eye Disease?
Often, individuals with Diabetic Eye Disease do not feel any pain or notice a change in vision. That’s why it’s critical to schedule an annual eye exam with your optometrist. Call your eye doctor right away if you notice one or more of the following symptoms:
- a significant increase in floaters – spots or dark strings
- dark, shadowy areas in the visual field or areas of vision loss
- wavy or blurry vision
- flashes of light
- frequent day-to-day changes in vision
- poor color vision
- Who is at high risk for Diabetic Eye Disease?
Anyone — and everyone — with diabetes is at risk for developing Diabetic Eye Disease. If your high blood sugar is not well-controlled, your risk increases. Also, the longer you have diabetes, the greater your risk for vision problems. More than half of patients experiencing diabetes will develop diabetic retinopathy.
- How does my optometrist diagnose Diabetic Eye Disease?
Your optometrist may place dilation drops in your eyes to expand the pupils of the eyes. This gives them a better window to examine a larger portion of the back of your eye with a magnifying lens to look for blood vessel damage. Your doctor will check both your vision and the pressure in your eyes.
Patients experiencing diabetes are at a higher risk of developing eye diseases that can cause permanent vision loss and should see their optometrist regularly. Annual eye exams are a general best practice, but based on changes in your eyes, your optometrist may recommend more frequent eye exams.
Follow your optometrist’s guidance on how often your eyes should be examined, and if you notice changes in your vision, call your eye doctor.
- How can you prevent Diabetic Eye Disease from progressing?
Controlling blood glucose levels is the key to managing diabetic eye disease.
In short, concentrate on the ABCs of diabetic disease management:
A: Normalize your A1C and keep blood sugar under control
B: Monitor and manage Blood Pressure
C: Lower your Cholesterol —and quit smoking if you smoke.
Commit to getting more physical activity. Ask yourself: How can I get more steps today? And, monitor your diet. Choose low glycemic index foods and drink water instead of sugary beverages. Take prescribed medications, and monitor blood sugar levels and blood pressure.
Your optometrist may prescribe medications to inhibit new blood vessel growth in the eye or stop fluid leaks. Additionally, laser treatments for leaky blood vessels can aid in slowing the progression of diabetic eye disease.
It’s never too late to begin taking better care of your health in general and to protect the health of your eyes. Start today!
Your eye doctor is your partner in helping you protect and maintain optimal eye health. Call us today to schedule your comprehensive eye exam.